Across Asia, patients with type 2 diabetes mellitus are characterised by a lower body mass index (BMI) and a higher prevalence when compared to Western countries (Chan, 2013; Ma and Chan, 2013; Hsu et al, 2015). In 2019, the prevalence of diabetes in Japan was reported as 19.7% in men and 10.8% in women, with a total of 11 million people suspected of having diabetes according to the Ministry of Health, Labor and Welfare Of Japan (Tomikue, 2023). The incidence of diabetic foot ulcers (DFUs) and amputations were reported to occur in 2.9 and 0.47 per 1000 person-years, respectively (Iwase et al, 2018). As the number of people with diabetes increases, so will the number of DFUs and potential amputations. While lifestyle changes are being encouraged, it is inevitable that better wound care techniques and products will be needed to maintain these patients’ productivity and quality of life.
Patients with a DFU face a decreased quality of life with 40% ulcer recurrence rates (Armstrong et al, 2017), challenges with mobility, the risk of infection, amputations and a shortened lifespan (Armstrong et al, 2017; Amstrong et al, 2020). Up to 85% of amputations may be avoidable with a holistic multidisciplinary team approach that incorporates innovative treatments and adherence to treatment parameters (Driver and Leon, 2021). Limb salvage should be a primary goal for the increasing population of patients with non-healing wounds.
The reconstructive ladder, as applied by the specialty of plastic surgery, focuses on the least invasive and reliable option for closing a soft tissue defect. When the most reliable option on the reconstructive ladder is unavailable, creative solutions for wound closure are required.
The following clinical reports present the first cases in Japan using a dehydrated human amnion/chorion membrane (DHACM) allograft (EPIFIX, MIMEDX Group, Inc, Marietta, GA, USA) as an adjunctive treatment to assist in closure of non-healing DFUs using a modified reconstructive ladder approach.
DHACM is an immune privileged, minimally manipulated and non-viable cellular human placental-derived tissue. The placental membrane [amnion/chorion] is immune privileged because it lacks antigens that elicit an inflammatory immune response in an immunocompetent host, as opposed to a transplant graft, which leads to rejection unless the immune system is suppressed. The mechanisms of action for DHACM have been highlighted in in vitro research and animal models. DHACM can provide an initial collagen scaffold barrier to support an environment conducive to granulation tissue formation (Bainbridge, 2013; Koob et al, 2013; Gonzalez et al, 2016). DHACM is known to contain over 300 identified preserved regulatory factors including epidermal growth factor, basic fibroblast growth factor, keratinocyte growth factor, transforming growth factor alpha and beta, vascular endothelial growth factor and tissue inhibitors of metalloproteinases, all of which in utero are essential to tissue generation (Koob et al, 2013; Lei et al 2017). Multiple prospective randomised controlled trials (RCTs) have shown that DHACM achieves 70–90% DFU closure rates within 6 to 12 weeks, which is significantly better when compared with standard wound care, and up to 96% closure rates when a placental-derived allograft is used concurrently with appropriate routine sharp debridement (Zelen et al, 2013a; Zelen et al 2013b; Zelen et al 2014; Tettelbach et al, 2019a; Tettelbach et al, 2019b). Large retrospective Medicare studies demonstrated improved closure rates when using a skin substitute compared with standard care (Armstrong et al, 2021) and that DHACM was cost-effective at any willingness to pay (Tettelbach et al, 2022).
Methods
Three patients with non-healing wounds were presented to health professionals in a hospital setting, both inpatient and outpatient. Informed consent was obtained from all participants. All procedures were performed in accordance with the ethical standards of the respective institutions involved and the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Wounds that remained refractory to closure were cleansed and surgically debrided in order to prepare the wound bed to receive a DHACM allograft. The allograft was trimmed to fit the wound bed, with one to three millimetres of overlap beyond the wound margins if possible. To facilitate adherence and incorporation to the wound bed, the DHACM was moistened with sterile normal saline only after placing the allograft over the wound bed. To secure the DHACM in place, a soft tack non-adherent dressing is recommended to be applied over the DHACM, with the aim of reducing the risk of the DHACM from being pulled off the wound bed whenever the outer secondary dressing requires changing. A fenestrated or mesh non-adherent dressing can also be used with, the added benefit of allowing free passage of exudate into the secondary dressing, thus potentially reducing the risk of maceration. To further secure the non-adherent dressing, use tape (Steri-Strips or Medipore, 3M ) to adhere the edges to the periwound region. Once the secondary dressing, such as hydrophilic foam, was applied over the DHACM, the portion of the affected extremity was then wrapped with a bandage (Coban or Ace, 3M) to bolster the DHACM onto the wound bed. Patients were asked not to disturb the wound for at least seven days, assuming low to moderate exudate, while the DHACM covering remained in place. Patients typically returned to the clinic within 7 to 14 days after the DHACM application for the next treatment until resolution. Cases were reviewed retrospectively.
Case 1, Diabetic foot ulcer
A male in his mid-forties with type 2 diabetes required amputation of the right great toe secondary to gangrene. Postoperatively, the patient presented to Fukuoka University Hospital with a 2cm x 2cm open wound over the amputation site (CASE 1A). At the time of the patient’s first visit (day 0) to the department of plastic, reconstructive and aesthetic surgery, signs of infection in and around the wound site had already improved and granulation tissue was present and healthy, yet the trajectory towards wound closure had stalled. Therefore, a DHACM allograft was applied over the open wound, rehydrated with sterile normal saline and secured in place after preparing the wound bed via sharp debridement. After 16 days of advanced treatment with a combination of standard care and four separate applications of DHACM, there was a significant reduction in wound surface area (Case 1B). Once the trajectory toward wound closure had been re-established, the ulcer progressed with standard care alone and flattened by the fourth week. Wound closure was confirmed in the sixth week (day 42) of treatment (Case 1C).
Case 2. Chronic ulcer
A male in his eighties with diabetes was transferred from another medical facility to the clinic at Oita Oka Hospital. The patient’s past medical history included a remote amputation of the left 5th toe. Before presentation, the patient developed a 3cm x 2cm non-healing ulcer on the posterior aspect of the left heel (Case 2A). Six days later (Case 2B and 2C), following debridement, the first DHACM application was made. The DHACM was subsequently bolstered with negative pressure wound therapy (NPWT) set at 75mmHg (Case 2D). One week after the first DHACM application and debridement, a second application was applied, and offloading was initiated. The DFU showed significant signs of improvement on the day of the third DHACM application, with an overall reduction in size and an increase in healthy granulation tissue in the ulcer base (Case 2E). Five applications were made over the course of 30 days in preparation for a full-thickness skin graft (FTSG) procedure. After 41 days, the nearly closed wound was debrided, and the FTSG was sutured into place (Case 2F and 2G). After a further six days, the graft had taken well and the patient was ambulatory (Case 2H). On day 47 the patient was transfered back to the originating healthcare facility for further rehabilitation.
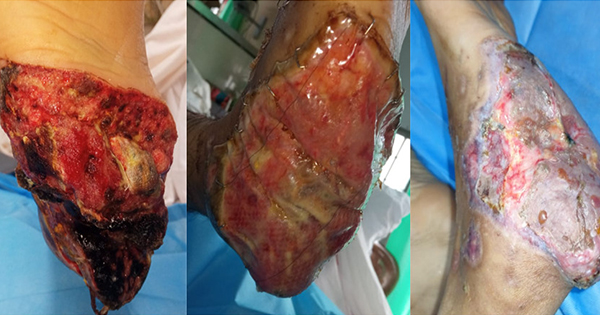
Case 3, Gangrene of the left foot
An elderly man in his early eighties was transferred to Tokyo Medical University Hospital for treatment of left foot gangrene (Case 3A) and chemotherapy. He had type 2 diabetes, chronic limb ischaemia that required an endovascular intervention and a metastatic intrahepatic neoplasm. The patient had developed a DFU of the left great toe that had progressed to gangrene, necessitating amputation of the 1st, 2nd and 3rd left toes in an attempt to salvage the foot. In week two, a wound culture revealed methicillin-resistant Staphylococcus aureus (MRSA), for which the patient was prescribed an antibiotic. After one month of conservative wound care, the DFU failed to close appreciably. Therefore, DHACM was initiated in an attempt to accelerate the wound’s closure process (Case 3B). Approximately one week after the first DHACM application over the DFU base, new granulation tissue was observed covering the exposed bone (Case 3C).
Encouraged by the postive response to the placental-derived allograft covering, the patient was treated weekly with sharp debridement, an NPWT device to bolster the allograft to the wound bed while concurrently providing moisture management for two weeks, and five weeks of DHACM appications (Case 3D). The DFU showed weekly reductions in wound surface (Case 3E and 3F). By day 90 and after six applications of DHACM, full wound closure was achieved (Case 3G).
The degree of wound closure achieved by this patient with exposed deep structures in the DFU base after starting DHACM allowed the attending physician to avoid a potentially painful and costly procedure such as a tissue transfer flap or a split-thickness skin graft.
Discussion
Non-healing wounds present a variety of limb preservation challenges that sometimes do not seamlessly fit the rungs of the traditional reconstructive ladder in Plastic Surgery. Here we presented three cases treated at various hospitals in Japan of increasing complexity that demonstrated the value of including DHACM in the spectrum of closure options. DHACM provides a barrier for non-healing DFUs and has been shown to significantly aid in resetting the wound bed environment, facilitating the wounds trajectory to proceed towards closure (Zelen et al, 2013; Zelen et al 2013b; Zelen et al 2014; Lei et al, 2017; Bianchiet al, 2018; Tettelbach et al, 2019a; Tettelbach et al, 2019b; Armstrong et al, 2021; Tettelbach et al 2022). Many clinical examples have been published in which the use of DHACM improved the reconstructive ladder in situations where surgical options for wound closure were limited. In select limb salvage cases, wound bed preparation by secondary intention becomes the only viable option to reach the next reconstructive rung (Thornburg et al, 2021; Ohara et al, 2022).
Preliminary clinical experience with DHACM in treating non-healing DFUs in Japan’s healthcare population has demonstrated that it is a promising alternative to tissue transfer flaps, skin grafts or other techniques for secondary intention resolution of extremity wounds with exposed bone and other deep structures. Additional studies and cases are needed to determine whether the use of DHACM improves patient outcomes when compared to the established wound care techniques currently practiced in Japan within the specialty of plastic, reconstructive and aesthetic surgery.