1 Cellular tissue changes from pressure and shear are not visible to the naked eye.
The cellular level changes lead to inflammation and oedema, due to an abnormal increase of interstitial fluid at the area of injury. The reperfusion of blood into an ischaemic area leads to erythema and elevated temperature from the increased blood flow (Oliveria et al, 2017).
2 The European Pressure Ulcer Advisory Panel (EPUAP)-National Pressure Injury Advisory Panel (NPIAP)-Pan Pacific Pressure Injury Alliance (PPIA) international guideline on pressure injury prevention recommends the use of temperature and subepidermal moisture as methods to detect early changes in skin due to pressure (EPUAP et al, 2019)
Detecting pressure damage early can prompt interventions to improve perfusion and reduce harm. The condition of skin and underlying tissue can serve as an indicator of early signs of pressure damage, therefore, routine augmented skin assessments provide an opportunity for early identification and treatment of skin injury, especially pressure ulcers.
3 The degree of ischaemia in skin and soft tissue can be measured by thermography.
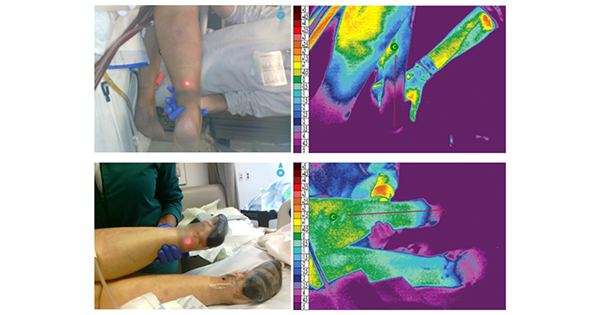
Perfusion of the skin is reflected in its surface temperature. Long-wave infrared thermography (or thermal imaging) measures the temperature of the skin and underlying soft tissues. When a control area is used for comparison, the difference in skin temperature between the control and involved areas can be objectively measured. The ischaemia of the tissues subjected to pressure, when present on admission to the hospital, verify that the pressure injury started prior to admission to any new level of care. Thermographic images of ischaemia from vasopressors not visible initially to the naked eye are visible on thermography with marked temperature loss. [Figure 1]
4 The degree of subepidermal moisture (SEM) can be measured by subepidermal moisture scanners.
Inflammation is the body’s first response to tissue damage and a mechanism to recover ischaemic injury. The inflammation increases vasodilation and permeability of capillaries, leading to leakage of plasma and creating localised oedema in interstitial spaces of the dermis (Okonkno et al, 2020). The SEM scanner detects changes to a tissue depth of about 4 millimetres (Gefen, 2018). Subepidermal moisture accumulation in the sacrum and heels can be measured and compared to surrounding areas, which were not exposure to pressure. An elevated amount of moisture (more than 0.6 from other tissue) signals risk. SEM is measured daily; the exact number of days is not defined. Recordings of delta (changes) can be entered into a graph for ongoing analysis [Figure 2].
5 You might hear that SEM measures Biocapitance
Biocapitance is the property of the tissue to store electric charge. The capacitance of tissues, called ‘biocapacitance’ because they are in tissues, is strongly affected by the amount of fluid in the tissue. SEM measurement technology captures the skin’s capacitance (ability to hold an electrical charge) by determining its relative dielectric constant (eg, electrical field resistance). SEM scanners measures tissue dielectric properties from an localised electrode placed on the skin, which records changes in biocapacitance (Moore et al, 2017).
6 Thermography and SEM provide accurate readings across skin tones.
Detecting erythema in darkly pigmented skin (Monk levels 9, 10, Fitzpatrick level 6) requires technology. Both thermography and SEM provide accurate data on early ischaemic and inflammatory changes in the skin due to pressure (Asare-Biaden et al, 2024).
7 Thermography can provide evidence of vasopressor-induced ischemia.
A common concern in the critically ill patients on vasopressors is the amount of vasoconstriction in the periphery. Risk factors for severe tissue ischaemia requiring amputation are duration of use and use of vasopressors with alpha-adrenergic activity (norepinephrine and phenylephrine) [Figure 2].
8 Ultrasound can detect early deep tissue pressure injury (DTPI)
Since its development in the 1970s, healthcare providers have used ultrasound as a diagnostic tool for a variety of conditions. The technology relies on pulsed sound waves emitted from a probe to penetrate the skin’s surface and determine its underlying structure based on the echo received from reflected waves. In the ultrasound images, structures with a greater density appear bright indicating higher echogenicity (hyperechoic). By comparison, areas of fluid or macroscopic oedema appear dark (hypoechoic). Intermediate-frequency (10-MHz) ultrasonography can detect various tissue patterns and possibly predict the fate of the DTPI. Unclear layered structures and hypoechoic lesions were more commonly seen in deep tissue pressure injury. Discontinuous fascia and heterogeneous hypoechoic areas are more reliable predictors of future evolution of the DTPI to more significant wounds. When ultrasound is combined with thermography, early forms of DTPI can be more accurately predicted (Aoi and Higashino, 2009).
9 Bruises can be detected using yellow and orange light sources in dark skin tones
Bruises are commonly confused with early deep tissue pressure injury. However, bruises form from haemoglobin breaking down through enzymatic processes in the extravascular space. There are coloured goggles and camera lenses that can be used to block the reflected light allowing the absorbed light to appear darker by comparison (Scafide et al, 2020).
10 Act on your findings by starting preventive interventions.
It is known that clinical assessment tools, such as the Norton and Braden scales do not accurately predict risk in all populations. Even clinical judgement does not always detect risk. Studies confirm that when elevated SEM readings were used to initiate a prevention bundle, pressure injury rates went down (Avsar et al, 2024). Likewise, thermographic findings showing altered perfusion can also prompt interventions and significantly reduce pressure injury rates (Simman and Holster, 2022).