Chronic wounds, such as diabetic foot ulcers, venous leg ulcers and pressure injuries, present significant clinical challenges due to their prolonged healing times and increased risk of infection. These complex wounds often occur in patients with underlying conditions, such as diabetes, hypertension and vascular insufficiency, which impair the body’s natural healing processes. Effective management requires a multidisciplinary approach that includes surgical interventions like debridement and amputation, along with advanced wound dressings and constant monitoring to prevent complications. Chronic wounds are persistent and difficult to manage for both patients and healthcare providers, largely because of the extended treatment periods needed. These wounds typically result from disruptions in the normal wound healing process, leading to long recovery times.
Healing challenging wounds poses a significant obstacle for both patients and healthcare professionals, as it often requires extended treatment. These difficult-to-treat wounds occur when the normal progression of wound healing is disrupted, leading to delayed recovery (Han and Ceilley, 2017). Several factors can hinder the healing of wounds, including the patient’s underlying health conditions, the characteristics of the wound itself (such as its size, duration and location), the type of clinical care provided and other physiological factors (Dowsett et al, 2015).
A fundamental distinction exists between the physiological processes and healing trajectories of acute and chronic wounds. Notably, chronic wounds are characterised by a persistent failure to progress through the typical stages of wound repair, a phenomenon often attributed to dysregulated inflammation and aberrations within the extracellular matrix (ECM; Eming et al, 2007; Schultz and Wysocki, 2009). Unlike acute wounds, which exhibit a controlled and time-limited inflammatory phase, chronic wounds are marked by an extended inflammatory response, potentially driven by an overabundance of infiltrating neutrophils (Menke et al, 2007). These neutrophils, while essential for initial defence against pathogens, release a plethora of proteolytic enzymes, including elastase, which possess the capacity to degrade crucial growth factors necessary for tissue regeneration.
Consequently, excessive levels of neutrophils engenders an imbalance between these enzymes and their physiological inhibitors, perpetuating the inflammatory phase and hindering the orderly progression of healing. This prolonged and unresolved inflammation significantly disrupts the delicate micro-environment of the ECM, which serves as a critical scaffolding structure and provides essential biochemical cues imperative for successful tissue regeneration (Haraway, 2006).
Heparan sulfates, a family of complex, high-molecular-weight polysaccharides, constitute a substantial component of the ECM and play a pivotal role in safeguarding and spatially organising the biochemical signals required for normal wound healing. However, in the context of an uncontrolled inflammatory response, the enzymatic activity of neutrophils leads to the degradation of these heparan sulfates, thereby compromising the structural and functional integrity of the ECM. As a result, the cells within the wound bed are no longer able to maintain a healthy and supportive ECM, which is essential for orchestrating the complex cellular processes involved in tissue repair and regeneration (Olczyk et al, 2015).
A primary goal in managing chronic wounds is to prevent and treat infection, along with removing dead tissue. The damaged skin barrier in chronic wounds makes them highly susceptible to infection, which can further delay healing. Debridement, the removal of necrotic tissue, is crucial for exposing healthy tissue and promoting the growth of cells needed for tissue regeneration and wound repair.
CACIPLIQ20® (OTR3) — a bioengineered analogue of heparan sulfate glycosaminoglycans — is a novel therapeutic agent known as a ReGeneraTing Agent (RGTA). It is a commercial name for a skin-adapted RGTA-based product to treat chronic wounds. It is a chemically engineered polymers that are designed to replace degraded heparan sulfate in the injured ECM. It protects naturally existing structural and signalling proteins by sequestering proteins through low-affinity binding, allowing for faster and high-quality tissue repair (Barritault et al, 2017). This technology offers a minimally invasive approach to regenerative medicine. RGTAs replenish depleted heparan sulfate, restoring the ability of the ECM to support cell adhesion, migration and differentiation. This also protects growth factors, cytokines, and chemokines from degradation, supporting tissue repair and regeneration (Barritault et al, 2011). Maintaining this signalling environment is crucial for effective tissue repair.
Additionally, CACIPLIQ’s heparan sulfate biomimetics directly interact with ECM glycoproteins like collagen, elastin and laminin. This binding is essential for crosslinking these structural components and creating a strong ECM scaffold. This scaffold provides the support and biochemical signals needed for tissue granulation and epithelialisation, fundamental processes in wound healing. Restoring this structural framework ensures cells can adhere, migrate, and differentiate properly, leading to successful tissue repair.
CACIPLIQ20 contains OTR4120, a specialised RGTA formulation for skin and plastic surgery (Barritault et al, 2011). A notable feature of RGTA is that they are able to protect and potentiate signalling peptides and growth factors, thereby re-establishing the ECM communication network. RGTAs are able to bind numerous heparin-binding growth factors, including FGF,19 VEGF12 and TGF beta 19, or chemokines, such as SDF-120, and, in doing so, protect them from proteolytic degradation and increase their bioavailability (Tong et al, 2009)
Chronic wounds, especially in diabetes, often heal poorly due to ECM dysregulation. In chronic wounds, the ECM is often degraded, hindering healing. RGTAs like OTR4120 in CACIPLIQ20 mimic molecules critical for ECM integrity and cell signalling. The specificity of OTR4120 for skin applications suggests a formulation tailored to skin regeneration, potentially optimising interactions with specific growth factors and ECM components (Ahmad, et al, 2018). This targeted approach makes CACIPLIQ20 a promising intervention for wound closure and tissue regeneration.
A single press of the spray delivers 140 µl of CACIPLIQ20 (sprayed from 5 cm perpendicular to the wound surface), which is sufficient to saturate the binding sites on 7cm2 of the wound surface. The spray format is significantly more user-friendly than the gauze compress delivery method. One vial can deliver up to 54 presses, can be used for the same patient or multiple patients and remains sterile for up to 6 months.
Methods
The case series study took place in Wound Care Clinic Hospital Kuala Lumpur, Malaysia, between July 2024 and March 2025. It involved patients who had chronic, non-healing wound. A convenience sampling method was used for this case series. All were treated with CACIPLIQ20 after the initial treatment methods failed or no alternative acceptable treatment was found. Inclusion criteria were patients with wounds that were present for more than 3 months. Most (90%) of the patients included had diabetes.
This case series was carried out in accordance with the Declaration of Helsinki guidelines and approved by the hospital’s review board. Patients gave consent to use clinical images and case details for publication/research purposes before the start of the study.
All patients underwent the same procedure in the clinic and were treated by nurses. All wounds were rinsed with sterile water. The wound was debrided accordingly. Treatment included two applications of CACIPLIQ20 per week, applied as the primary dressing.
The secondary dressing depended on the amount of exudate. The wound was secured with gauze and bandage. The dressings were changed three times a week until the end of the study. Offloading with paddings was used for DFUs, while two-layer compression treatment was used for the patient with a venous leg ulcer (VLU). No other advanced dressings that could alter the healing times were employed for this study.
The cases were followed from initial use of CALCIPLIQ20 to discharge, assessing treatment efficacy using wound size. The wound was continuously assessed via Tissue, Infection, Moisture and Edge of Wound (TIME) assessment (Nair et al, 2021) and the periwound skin assessed using Harikrishna Periwound Skin Classification (HPSC; Nair et al, 2020).
The wound bed was described and any changes from baseline wound appearance were documented on every visit to allow determination of changes in healing rate and wound size. Comprehensive monitoring, tracing the process from inception to discharge, predominantly relied on wound size as the key efficacy metric. Measurement of wounds (length × width) and their progress was assessed every time the dressing was changed.
Results
We recruited 10 patients, nine men and one woman [Table 1] with various comorbidities, including diabetes (n=9), hypertension (n=7), and hyperlipidaemia (n=4). Five patients had DFUs and the others had different conditions – pressure injury, VLU, carbuncles and an infected wound.
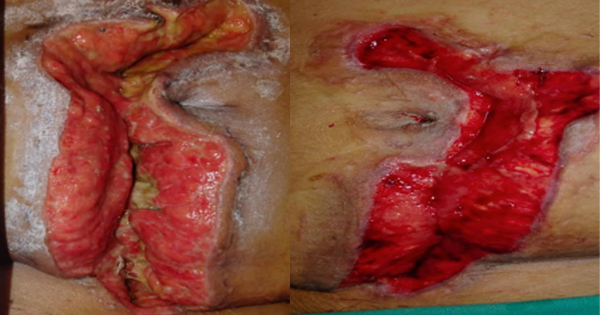
The 10 cases are shown in Figure 1. By the end of the study, all wounds had healed completely.
Figure 2 demonstrates CACIPLIQ20’s potential in managing chronic wounds, with healing achieved across a spectrum of wound ages, albeit with longer durations required for older wounds. It supports the hypothesis that early intervention may result in quicker wound closure, although the therapy remains beneficial even in advanced cases.
Discussion
In these cases, we had the opportunity to use a novel matrix therapy agent in the field of regenerative medicine, CACIPLIQ20, also known as a RGTA.
CACIPLIQ20 has a simple and conservative mode of action. Its ability to specifically localise to sites of injury throughout the restoration process, with no evidence of toxicity, makes it a safe-profile product. For CACIPLIQ20 to penetrate the wound thoroughly and demonstrate its full effects, rigorous debridement must be performed before application of CACIPLIQ20. The speed of healing from CACIPLIQ20 to complete closure also reduces the rate of complications such as infections, hospitalisation and amputation, thus improving overall quality of life for patients (Langer and Rogowski, 2009).
Regardless of wound size and type, the results from these 10 patients have shown CACIPLIQ20 has assisted in complete wound closure for non-healing wounds. Wound healing was observed in all patients, with the quickest of 28 days in patient 1.
CACIPLIQ20 led to a significant decrease in wound size, after 28–90 days, and this was associated with increased granulation tissue. All the wounds had completely healed.
In long-term follow-up of the patients, no reopening of closed ulcers was observed, and no amputations were performed because of ulcers.
Patients with chronic wounds experience excruciating pain, thus decreasing quality of life. In 2008, Barritault et al reported that at 1 month post application of CACIPLIQ20, 80% of ulcers improved, with a reduction in size of 12%–100%, good tolerance and reduced pain (Barriault et al, 2008).
A similar study carried out in an underserved metropolitan area on patients with chronic ulcers ranging in duration between 2.5 and 10 years showed 22% of the participants had complete wound closure in 1 month (Desgranges et al, 2011)
Wound-related pain can be measured via wound pain scale and visual analogue scale. Desgranges et al (2011) noted that patients experienced significant pain relief because of healing. This correlates with our study, where the pain score was reduced for the eight patients in whom pain was measured, with initial scores of 2–4 reducing to 0 for all eight with CACIPLIQ20 treatment.
Irving’s 2019 study has shown that CACIPLIQ20 is cost effective because faster healing leads to less time required for wound management by healthcare practitioners in addition to decreasing treatment costs, faster wound closure also relieves the physical and emotional burden of non-healing chronic wounds, improving quality of life (Irving, 2019)
Limitations
Our case series has several limitations. First, we had no control group. A larger study will be required to increase the reliability and generalisability of the study. The lack of an adequate control group and the great heterogeneity of the variables may prove to be an important bias, requiring further studies with more robust evidence.
Conclusion
Wound healing normally occurs in a predictable sequence; however, in some instances healing is prolonged or never achieved. The healing process is a complex interaction involving patient- and wound-related factors, the treatment used, and the skills and knowledge of healthcare professionals.
We would like to highlight the uniqueness of CACIPLIQ20 as a regenerative agent: its ease of use, acceleration of the healing process, replacing like for like tissue and reducing pain. In the present case series, all the patients had experienced delayed wound closure before CACIPLIQ20 treatment, however, all wounds closed fully after initiation of treatment with CACIPLIQ20 independent of aetiology.
CACIPLIQ20 has potential as a strategic intervention for various types of chronic wound. Its capacity to transform wound care underscores the urgent need for in-depth exploration of its potential and application.
While these cases substantiate the efficacy of the innovative approach, broader validation necessitates expansive case series and rigorous studies. This case series depicts adequate evidence in support of the use of this RGTA