Aortoiliac occlusive disease is a type of peripheral artery disease that specifically impacts the infrarenal aorta and the iliac arteries. This condition leads to reduced blood flow due to narrowed lumens or the embolisation of plaques, which affects the organs located further downstream. Symptoms can vary widely, ranging from no symptoms at all to severe limb-threatening or even life-threatening situations (Heaton and Khan, 2024). Critical limb ischaemia is a medical condition characterised by ischaemic pain while at rest or the presence of tissue damage, including non-healing ulcers or gangrene, associated with peripheral artery disease. This condition is classified according to the Trans-Atlantic Inter-Society Consensus (TASC) system, which takes into account the severity, location and size of the stenosis. Management recommendations can be tailored based on these classifications. Previously, open surgical treatment was the primary treatment from the past for TASC II C/D. Currently, endovascular procedures are advised for complex aortoiliac occlusive disease (AIOD) and cases with a higher risk of complications with open surgical treatment. This recommendation is based on the lower rates of morbidity and mortality associated with these procedures, as well as improved long-term outcomes (Bontinis et al, 2024).
The severity of AIOD is classified according to the TASC system, which categorises the condition into different types based on the location and severity of the stenosis:
- TASC A: Small, focal lesions suitable for percutaneous interventions.
- TASC B: More extensive lesions that may require a combination of endovascular and surgical approaches.
- TASC C and D: Complex lesions involving long segments or severe occlusions, traditionally managed with open surgical procedures.
Case presentation
A 94-year-old Filipino woman, a retired secretary, presented with a 3-month history of a non-healing wound. She initially presented with superficial abrasions with noted bleeding from an incident where her pet dog accidentally stepped on her foot. There had been no previous consultation or medication prescribed. According to the patient, the lesion had not increased in size, but was noted to have hyperaemia and dark discolouration over time associated with intermittent pain on the left leg. Due to the persistence and progression of the wound lesion, the patient sought a consultation from a known doctor, and was given antibiotic creams, which they applied directly to the wound, which they applied directly to the wound.
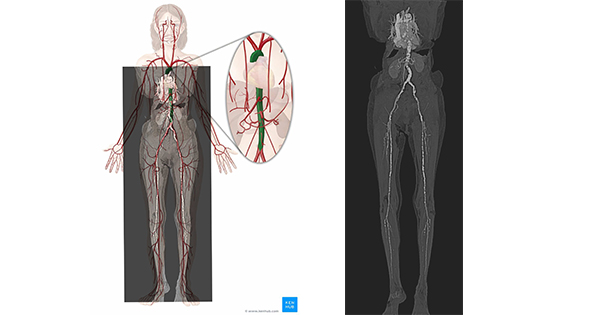
The patient was then referred to a wound specialist, and an arterial and venous duplex scan was done, showing peripheral arterial occlusive disease. The patient was referred for peripheral angioplasty. She has hypertension and takes amlodipine regularly, but with no diabetes. She also has congenital deafness. Her paternal and maternal sides of the family have a history of hypertension and diabetes. She is a non-smoker and a non-alcoholic beverage drinker. On physical examination, she was conscious, coherent and not in distress with vital signs as follows: prehypertensive at 130/90 mmHg, non-tachycardic 85 beats/minute, non-tachypneic 20 cycles/minute, afebrile 36.5°C and with normal oxygenation of 98%. She has a 2 cm × 2 cm eschar at interdigital area third to fourth digit on the left foot, gangrenous fourth digit left foot, hyperaemic area on the left foot [Figure 1], no oedema, bilateral lower extremity cold to touch, left femoral pulse, popliteal, dorsalis pedis — unappreciated, right femoral pulse, popliteal, dorsalis pedis – (+)1.
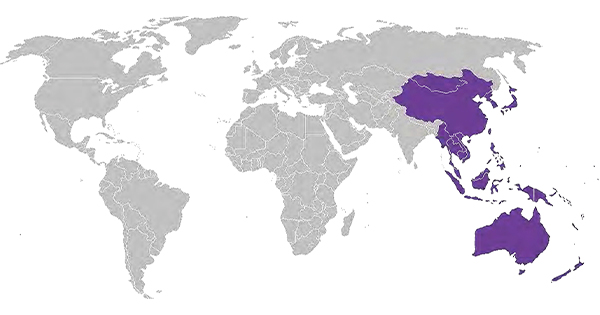
On the second hospital day, the patient was referred to the thoracocardiovascular surgery service for possible peripheral revascularisation. CT aortogram and peripheral angiogram [Figure 2], which showed extensive intimal calcifications in the thoracic, and abdominal aorta, both common iliac arteries, both internal and external iliac arteries, and short segment critical stenosis in the infrarenal segment of the abdominal aorta secondary to a central obstructing densely calcified thrombus, which prompted initial plan for peripheral angioplasty.
On the 11th hospital day, intraoperatively, heavy calcification at the aortoiliac bifurcation was seen. The patient underwent peripheral angioplasty with aortoiliac artery stenting using a covered endovascular reconstruction of the aortic bifurcation (CERAB). The patient tolerated the procedure well with no intraoperative complications.
On the first postoperative day, the patient had stable vital signs, with no bleeding on the post-op site, with improvement of bilateral femoral pulses +2 from an unappreciable pulse on the left and +1 on the right. On the second postoperative day, the patient still has stable vital signs, still with good pulses and now with the absence of claudication. Discharge plans were given on the third postoperative day. On the fourth postoperative day, the patient was deemed fit for discharge. The patient was then sent home with a final diagnosis of a non-healing wound, the third to fourth digit of the left foot, secondary to AIOD.
Upon follow-up 1 month post-op, the patient was found to be apparently well without subjective complaints, with the absence of claudication and with delineation of gangrene limited only at the third and fourth digit of the left foot without progression.
Final diagnosis
For the case of our patient, the final diagnosis is a non-healing wound, third to fourth digit of left foot secondary to AIOD, hypertensive atherosclerotic cardiovascular disease, status postCERAB, and congenital deafness.
Treatment
Old age is a significant risk factor for aortoiliac occlusive disease due to the cumulative effects of atherosclerosis, reduced arterial elasticity, and comorbid conditions. For older patients with complex AIOD TASC C/D, such as our patient with classification of TASC D, CERAB offers a less invasive and effective alternative to open surgery. By addressing extensive occlusions and reducing the risks associated with traditional surgical approaches, CERAB can improve outcomes and quality of life for older individuals (Gabel et al, 2019).
The CERAB is an innovative technique designed to treat complex cases of AIOD. This procedure focuses on reconstructing the aortic bifurcation — the point where the aorta splits into the iliac arteries — using covered stents to address severe arterial blockages and restore blood flow (Radosa et al, 2022).
Outcome and follow-up
Upon discharge, the patient was advised to continue maintenance medications for her hypertensive atherosclerotic vascular disease and to do a follow-up check-up after 1 week for assessment of the post-op site and wound on the left foot.
Upon follow-up 1 month post-op, the patient was found to be apparently well without subjective complaints, with the absence of claudication and with delineation of gangrene limited only at the third and fourth digit of the left foot without progression.
Discussion
AIOD is a significant vascular condition that impacts the blood flow in the aorta and iliac arteries, which are critical for supplying blood to the lower limbs and pelvis. This disease is a form of peripheral artery disease and can lead to various clinical manifestations depending on its severity and the extent of arterial blockage (Heaton and Khan, 2024).
AIOD occurs when the lumens of the infrarenal aorta and iliac arteries become narrowed or blocked due to atherosclerosis, which is the build-up of fatty plaques. This obstruction reduces blood flow to the lower extremities, resulting in ischaemia and potential damage to tissues and organs further downstream. The condition can be exacerbated by factors, such as diabetes, hypertension, smoking and hyperlipidaemia (Heaton and Khan, 2024).
Symptoms of AIOD can vary widely. Patients can be symptomatic with no noticeable symptoms despite significant arterial blockage. Others may have pain, cramping, or weakness in the legs during physical activity, which typically resolves with rest. In more severe cases of critical limb ischaemia, patients might have rest pain, ulcers or gangrene, which can lead to limb-threatening situations.
AIOD can be diagnosed through a combination of clinical evaluation and imaging studies. Key diagnostic tools include: ankle-brachial index: a non-invasive test that compares blood pressure in the ankle with that in the arm to assess the degree of arterial blockage. Arterial and venous duplex ultrasound to visualise blood flow and detect plaque buildup. CT angiography or MR angiography provides detailed images of the arterial system to evaluate the extent and severity of the occlusion. Digital subtraction angiography is often used for planning interventional procedures due to its detailed visualisation of the arterial anatomy.
Management strategies are tailored to the classification that has been discussed. It could be a combination of lifestyle modifications, medications or surgical management. Addressing modifiable risk factors through smoking cessation, diet, and exercise is very important in patients with AOID. While symptoms and cardiovascular risk are managed through antiplatelet agents, statins, and medications for hypertension and diabetes. Traditionally, the main approach for complex cases (TASC C/D) is through open surgery, involving procedures such as bypass grafting to restore blood flow. Endovascular Interventions such as balloon angioplasty, stenting, atherectomy and CERAB are increasingly preferred for complex cases due to lower morbidity and mortality rates. Endovascular techniques have seen significant advancements, improving outcomes and expanding their use in complex AIOD cases. New technologies, such as drug-eluting stents and improved imaging techniques, have enhanced the efficacy and safety of these procedures.
A study in 2015 presented initial results for the CERAB technique, which aims to reconstruct the aortic bifurcation using covered stents in patients with aortoiliac occlusive disease. Between 2009 and March 2014, 103 patients (51 men, 52 women; median age 61 years, range 36–85 years) were treated with CERAB across two clinics. Lesion types included six TASC II B, nine TASC II C, and 88 TASC II D. Technical success was achieved in 95.1% of cases, with primary patency rates of 87.3% at 1 year and 82.3% at 2 years, and secondary patency rates of 95.0% at both 1 and 2 years. While the 30-day complication rate was 23.3% with no mortality, the CERAB technique shows promise as a safe and effective alternative to open surgical reconstruction, warranting further comparative studies with current standards (Grimme et al, 2015).
Another study, a 2-year retrospective analysis of patients who underwent CERAB for AIOD at San Giovanni Addolorata Hospital from January 2016 to December 2019, included 24 patients (14 men, 10 women; median age 59 years, range 37–79 years). The cohort consisted of 29.2% with TASC II C lesions and 70.8% with TASC II D lesions, primarily treated for intermittent claudication (75%) or critical limb ischaemia (25%). Technical success was achieved in all cases, with minor perioperative complications in 12.5% of patients, including one case of intraoperative iliac rupture. The median hospital stay was 2 days (range 1–9), and there were no perioperative deaths or mortality by the last follow-up. While CERAB demonstrated effectiveness and low complication rates at mid-term follow-up, further long-term studies are needed to validate its role as a primary treatment for extensive AIOD, though it may become a preferred option, especially in the context of current healthcare constraints (Borghese et al, 2022; Radosa et al, 2022).
AIOD is a complex condition with a range of clinical presentations and management options. While traditional open surgical approaches have been the cornerstone of treatment for severe cases, endovascular interventions are increasingly becoming the preferred choice due to their less invasive nature and favorable outcomes. A multidisciplinary approach involving lifestyle modifications, medical therapy and interventional procedures tailored to individual patient needs is essential for optimal management of AIOD.
Conclusion
The CERAB technique offers a less invasive approach to treating complex cases of AIOD, characterised by its low complication rate and shorter hospital stays. This method is particularly advantageous for managing late-stage AIOD or anatomically complex lesions, providing effective treatment with reduced operative risk, especially for older patients. As an endovascular procedure, CERAB can be a preferred choice for high-risk patients, delivering a safer alternative to traditional surgical approaches