The skin, the body’s largest organ, has regenerative abilities, but in severe cases, it cannot heal on its own. While autologous skin grafts are commonly used, factors such as poor physiological condition and large wound size in polytrauma patients often limit their effectiveness. This creates a need for alternative solutions.
Skin substitutes, which may be biological, synthetic, or biosynthetic, offer temporary or permanent wound coverage. They prevent fluid loss, support cellular infiltration and promote remodelling to restore tissue function. These substitutes range from autologous grafts to bioengineered options. At our centre, we routinely use spare-part skin grafts (i.e. preserved skin grafts harvested from amputated limbs), allografts, amniotic membranes and commercially available dermal templates. Dermal templates are collagen scaffolds or artificially constructed polymer scaffold that act as matrix for new tissue ingrowth. They also act as temporary physical barrier to prevent fluid loss and external pathogen invasion.
In this case series, we share our experiences with various skin substitutes in the management of polytrauma patients.
Apart from the skin substitute used, the rest of the wound care protocol was standardised across all patients. Wound cleansing and dressing were performed every 24 hours until the application of the skin substitute. Post-application, which was routinely coupled with negative pressure wound therapy (NPWT), the dressing was opened after 5 days. Wound cleansing was done using normal saline and Microdacyn Wound Care Solution (Te Arai BioFarma). All patients with soft tissue injuries were started empirically on intravenous Cefuroxime (Clindamycin in case of penicillin allergy), with the addition of intravenous Gentamicin in cases of open Gustilo-Anderson grade 3 fractures. Wound cultures were obtained on day 1, and antibiotics were subsequently tailored based on culture sensitivity results, usually within 72 to 96 hours.
These patients were managed by a multidisciplinary team comprising trauma surgeons, orthopaedic surgeons, critical care specialists, wound care nurses, and physiotherapists to ensure comprehensive care throughout their hospital stay.
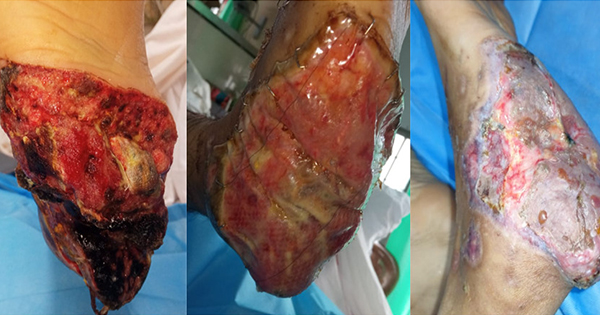
Case 1
A 28-year-old man in class 4 shock with pelvic fractures, multiple open long bone fractures, and right heel pad loss underwent damage control surgery and bilateral internal iliac artery ligation, followed by resuscitation in the ICU. He developed sepsis, requiring multiple debridements of the right heel.
Integra Dermal Regeneration Template (Integra Life Sciences, Plainsboro, NJ, US) with negative pressure wound therapy (NPWT) was applied, followed by a split-thickness skin graft (STSG; Figure 1). Integra, a dermal regeneration template, was chosen for its ability to cover exposed bone, ease of use and minimal donor site morbidity.
Challenges
Exposed calcaneus and tibial fracture, combined with sepsis, typically warrant amputation, especially in resource-limited settings. However, serial debridements and targeted antibiotics led to gradual improvement in this case.
Immediate coverage of the exposed calcaneus was critical to prevent osteomyelitis or osteonecrosis. STSG was not suitable due to exposed bone, and local flaps were avoided due to extensive leg contusions.
Case 2
A 10-year-old boy in class 4 shock, with complex pelvic fractures and multiple long bone fractures, failed to respond to crystalloid resuscitation and was taken for damage control surgery and bilateral internal iliac artery ligation. After stabilisation in ICU, a colostomy was performed due to perineal injury, and long bone fixation was completed.
The patient had extensive abrasions and friction burns on the right side of the body, managed with silver sulfadiazine dressing, while a skin allograft donated by his mother was applied to the right elbow. The allograft was used as a temporary measure to improve the wound bed and allow time for healing, making the patient ready for autografting once his condition stabilised. The graft was rejected after 3 weeks, but his general condition improved, and STSG was successfully performed [Figure 2].
Challenges
Autologous STSG was initially avoided in this case due to limited donor sites, extensive friction burns, the colostomy and his poor general condition.
Case 3
A 9-year-old girl sustained grade 4 renal, grade 3 splenic, liver and pancreatic injuries, with soft tissue loss on the right side of her face exposing bone, and large friction burns on the abdomen and forearms. She developed sepsis on day 2, and a thorough wound wash was performed with normal saline and Microdacyn Wound Care Solution.
On day 3, debridement and Endoform Dermal Template (Aroa Biosurgery, Auckland, New Zealand) dressing were applied to the facial wound, followed by hyperbaric oxygen therapy. Endoform, an extracellular matrix scaffold, was used to promote granulation and reduce the risk of osteomyelitis. It was chosen for its ease of use and minimal morbidity.
After 10 days, a STSG was performed, while the rest of her abrasions were treated with silver sulfadiazine dressings [Figure 3].
Challenges
- Early closure was essential due to the exposed bone, but the defect was too large for primary repair.
- Flap reconstruction was not viable due to her poor condition from sepsis and multiple organ injuries.
Case 4
A 29-year-old man with a crush injury to the right lower thigh underwent an above-knee amputation. Skin was harvested from the amputated limb. The patient later developed stump infection and wound dehiscence, requiring debridement and NPWT for 4 days. Preserved skin from the amputated part was successfully grafted over the stump 12 days post-harvest [Figure 4].
Challenges
- A large raw area over the stump could not be closed primarily after debridement, necessitating STSG.
- To avoid additional morbidity from fresh skin harvesting, the preserved graft from the amputated limb was used.
Case 5
A 31-year-old man with a pelvic fracture, bladder injury, bilateral leg fractures, and hypoxic brain injury was referred 5 days post-injury. He had a large Morel-Lavallée lesion over the left flank, gluteal region, and thigh, initially managed with drain placement. After skin necrosis developed, debridement was performed, but the wound bed showed insufficient granulation despite NPWT. The raw area was then treated with a BTM (Biodegradable Temporizing Matrix; PolyNovo, Port Melbourne, Australia) dressing, followed by STSG [Figure 5].
Challenges:
- The patient had a large raw area, poor general condition, and sepsis, necessitating early wound coverage. However, due to the wound being in a pressure area and lateral nursing being unfeasible because of pelvic and other fractures, early STSG was not an option.
- BTM was chosen to promote granulation and provide a physiological seal for the wound bed.
Case 6
A 32-year-old male presented in class 3 haemorrhagic shock with an open pelvic fracture, perineal injury, urethral injury, and degloving injury of the left lower limb. He underwent damage control surgery (DCS) and was shifted to ICU. Necrosis of the left lower limb skin required debridement.
On day 12, a meshed cadaveric skin allograft was applied to the lower limb and perineum [Figures 6 and 7]. An allograft was chosen as an early wound cover to prevent infection and fluid loss, given its cost-effectiveness compared to other skin substitutes.
Despite treatment, the patient developed septic shock and multi-organ dysfunction syndrome and died on day 57.
Challenges
The extensive raw area and poor systemic condition posed significant risks. The extensive raw area increased risks of infection, fluid and protein loss. Poor systemic condition further increased his susceptibility to infection and graft loss.
NPWT was unsuitable due to the wound’s size and anatomical location, making it difficult to maintain adequate pressure and seal.
As the area was very large, a living donor graft could not be taken and instead commercially available cadaveric skin allograft was used.
Discussion:
In India, extremity injuries are the second most frequent injury after head injuries (Kashid et al, 2020). Mangled limbs, degloving injuries and crush injuries account for a significant number of lower extremity injuries, most of which end up as non-healing wounds.
Normal wound and fracture healing processes require a well-balanced inflammatory response. In patients with polytrauma, wound healing is delayed, due to inflammatory dysregulation (Horst et al, 2020). Polytrauma is believed to cause alterations in local and/or systemic inflammatory responses, which are crucial in the early phases of fracture healing. (Horst et al, 2020) Additionally, factors such as hypoxia, hypoperfusion, poor nutrition, infection, oedema and shearing forces also contribute to delayed wound healing in trauma patients. Thus, a multidisciplinary approach is necessary for managing patients with soft tissue injuries. These patients were managed by a multidisciplinary team comprising trauma surgeons, orthopaedic surgeons, critical care specialists, wound care nurses, and physiotherapists to ensure comprehensive care throughout their hospital stay.
Primary closure is often not feasible in traumatic wounds due to their large size and contamination. Skin grafts are also prone to loss due to poor general conditions, exposed bones and tendons, and contamination. Autografts are generally avoided because of a high chance of graft failure and the creation of another wound, which can be a source of pain and infection, and affect nursing care.
An ideal dressing for large skin wounds should be non-antigenic, non-toxic, reduce water permeability, act as a barrier to microorganisms, minimise pain, adhere firmly, protect underlying tissue from additional trauma and be cost-effective and readily available (Rezvani Ghomi et al, 2019).
Skin allograft is a well-established technique for skin coverage in patients with extensive burns (Sheridan and Tompkins, 1999). However, Qaryoute et al. (2001) report that this is a temporary wound coverage technique, because graft rejection is likely to occur within a couple of weeks. Skin allograft can be used in polytrauma patients with large wounds to bridge the initial poor general condition of the patient and improve recipient bed status for definitive autografting. We use commercially available cadaveric skin graft or skin donated by close relatives. Skin grafts from related donors, may increase graft longevity, due to human leukocyte antigen compatibility (Gideroğlu et al, 2016).
Other traumatic wounds that are small in size but difficult to manage due to exposed bones and tendons include heel pad avulsions and soft tissue defects on the face. In these, flap cover is not an option because of associated injuries, systemic conditions, risk of failure, donor site morbidity and prolonged operation time (Janis et al, 2011).
Prolonged cortical bone exposure can result in dehydration and bone necrosis, leading to infection, osteomyelitis, and sepsis, which may necessitate amputation (Verhelle et al, 2003). Bellidenty et al. (2014) report that the success rate of free flap surgery for lower leg defects decreases to 73% when performed later after initial trauma.
In high-velocity injuries, post-traumatic vessel disease, i.e. trauma involving the vascular wall and perivascular tissues, reduces the availability of recipient vessels for free flap surgeries (Bellidenty et al. (2014). NPWT is a well-known wound bed preparation technique for exposed bones, but Verhelle et al (2003) note that the time required for large wounds is a major drawback.
To avoid open wounds with exposed bone, which increase the risk of wound infection, bone necrosis, and osteomyelitis, dermal substitutes were used for wound cover. Dermal matrices are now part of the new reconstructive ladder (Janis et al, 2011). Integra, BTM and Endoform are the dermal substitutes we use in our centre. The role of dermal matrices in avoiding free flap reconstruction or amputation in complex lower extremity burn reconstruction has been explored with good outcomes by Lee et al (2008). Although technically simpler, dermal matrices demand diligent wound care, with engraftment rates ranging between 35% to 96% (Heimbach et al, 1988; Machens et al, 2000). Complications include seromas, haematomas and infection. Dermal matrices are more labour-intensive, expensive, and time-consuming compared to single-stage flap reconstruction. However, Scalise et al. (2020) reported that they preferred them over flaps due to patients’ general conditions, to avoid prolonged surgeries and donor site morbidities. An overall complication rate of 10.8% has been reported in previous studies, though no predictors for complications were identified (Scalise et al, 2020).
Apart from the dermal templates mentioned above, we also have an experience of using MatriDerm (Dr Otto Suwelack Skin & Health Care AG, Billerbeck, Germany), a single-layer dermal substitute in salvaging crushed extremities [Figure 8].
Human amniotic allograft membrane (HAM) is a rich source of amino acids and growth factors that promotes wound healing by facilitating cell migration and repair (Thompson et al, 2019). Tseng et al. (1999) have shown that HAM also reduces the risk of fibrosis and thus scar formation.
We use cryopreserved amniotic membrane at our centre. A randomised feasibility study performed in our centre showed significant reduction in wound exudate, peripheral oedema and pain (Choudhary et al, 2023).
Recently, we began harvesting skin from amputated parts, preserving them in the refrigerator after wrapping in paraffin gauze. Prior to harvesting, amputated parts are thoroughly scrubbed, painted, and draped. We use these stored grafts within 2 weeks. Although there is no definitive consensus on the storage and usage of stored STSG, we find this to be a cost-effective, easy, and safe technique for wound coverage in polytrauma patients undergoing amputations. This technique allows us to avoid donor site morbidities and multiple surgeries, as the graft can be applied at the bedside.
Apart from these we also regularly use Fibroheal Ag (Fibroheal Woundcare Pvt. Ltd), a silk fibroin-based dressing, to accelerate healing in friction burns [Figure 9].
Conclusion
Management of soft tissue injuries is an arduous task. Assessment of the patient’s physiological condition is of utmost importance in determining the treatment plan for polytrauma patients. The nature of the wound bed plays a key role in deciding the means of wound coverage. We should always aim at eliminating donor site morbidities. Multimodality treatment must be employed.