Bioactive microfiber gelling (BMG™) dressing is a type of wound dressing material that is made of up 100% chitosan, a natural polysaccharide derived from natural resources including shellfish, mushrooms and insects. It is derived from deacetylated chitin with a minimum of 50% of its amine groups in the free form (Zhang et al, 2020). Chitosan has several characteristics that make it suitable for use as a modern dressing, such as antimicrobial, anti-inflammatory, low immunogenicity and antioxidant properties (Patrulea et al, 2015; Dragostin et al, 2016).
Chitosan exerts a beneficial impact on each of the four phases of wound healing. During the haemostasis phase, chitosan exhibits the capacity to absorb plasma, induce coagulation of erythrocytes, promote platelet aggregation and activate platelets. Red blood cells adhere to chitosan macromolecule chains, hence facilitating the haemostatic process (Whang et al, 2005). During the inflammatory phase, chitosan exerts an anti-inflammatory action via modulating the activity of tumor necrosis factor-alpha (TNF-α), which subsequently decreases the production of nitric oxide (Yoon et al, 2007). During the proliferative phase, lysozymes break down chitosan to create N-acetyl-D-glucosamine, which promotes the growth of fibroblasts and the formation and remodelling of collagen (Axio Biosolutions). Chitosan dressing also inhibits the metallo-matrix proteases (MMP 2 and MMP 9) that help to regenerate the extracellular matrix quickly. It also speeds up the granulation process in the proliferative phase (Archana et al, 2013). In the maturation phase, chitosan contains a component of N-acetyl glucosamine that helps to reduce scar formation (Nair et al, 2020).
Objectives
The aim of this case series is to discuss the efficacy of BMG dressings in facilitating wound healing in post-surgical wounds.
Method
This case series involved the application of a BMG dressing (MaxioCel®, CD Medical) on four patients. It was conducted in an outpatient setting at Wound Care Clinic (WCC) Hospital Teluk Intan. Table 1 illustrates the baseline demographic summary of enrolled patients. For all patients, the TIME concept was used to assess the wounds and Harikrishna Periwound Skin Classification (HPSC) [Table 1] was used to describe the periwound area. The wound was cleansed using a surfactant containing antimicrobial solution (Octenisept®, Schülke) and, as per the wound requirements, debridement was performed, prior to a BMG dressing being used. Once the tendon was almost closed, we initiated the BMG dressing usage. Gamgee roll was used in the outer layer as a secondary dressing and changed on a daily basis.
Ethical approval
Written consent from the patients for the use of patient details and photographs was obtained.
Results
Table 2 summarises the clinical outcomes, including the major observations and the key results of these clinical evaluations.
Patient 1: Postoperative wound secondary to infected left diabetic foot ulcer
This case involved a 52-year-old woman with pre-existing type 2 diabetes (T2D) . Initially, she presented with an infected diabetic foot ulcer that required wound debridement. She was referred to the wound care clinic (WCC) following her discharge for wound management. Figure 1 depicts the progression of wound healing during the treatment period. The wound had a 90.86% reduction in size after 85 days of treatment.
Patient 2: Postoperative wound secondary to infected left below-knee amputation stump
This case centred on a 56-year-old man with pre-existing T2D, hypertension and dyslipidaemia, who underwent left below-knee amputation due to wet gangrene in sepsis. The patient’s blood glucose levels were challenging to manage in the hospital ward as a result of infections. He had to undergo repeated wound debridement procedures for his stump. The results of the tissue culture revealed the presence of Pseudomonas aeruginosa, which was then treated with appropriate antibiotics based on the wound’s sensitivity. Subsequently, he was referred to the WCC to continue his wound treatment. Figure 2 shows wound size reduction by 92.42% from initial wound size after 41 days of treatment using BMG dressing.
Patient 3: Postoperative wound secondary to left eye fungating squamous cell carcinoma.
This case is a 73-year-old man with pre-existing hypertension who was diagnosed with left lower eyelid basaloid squamous cell carcinoma in 2019. He defaulted on his treatment and follow-up for the previous 2 years. He returned in November 2023 for a fungating mass with maggot infestation over his left eye. The left eye exenteration was performed at Serdang Hospital, Malaysia, within the same week. He was then referred to WCC for wound management for his left eye. Figure 3 illustrates the wound progression throughout the treatment in which wound size was reduced by 58% in 63 days.
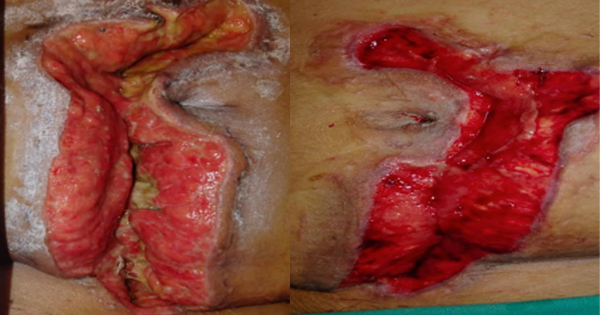
Patient 4: Postoperative wound secondary to left hand necrotising fasciitis
A 69-year-old man with newly diagnosed T2D was admitted for sepsis secondary to left hand necrotising fasciitis. He had extensive wound debridement and ray amputation of his left thumb. Subsequently, he was referred to the WCC for his post-surgical wound. Figure 4 demonstrates the wound healing progress where his wound reduced by 89.71% from initial wound size in 73 days.
Discussion
In this case series, all four patients were treated using a BMG dressing, which is commonly used for a variety of wounds at different anatomical sites.
Although BMG dressing can be used in combination with other wound care products, this study focused on the use of BMG dressing alone to assess its individual efficacy. The dressing also conforms to the wound bed, is easy to apply and can be removed without the patient experiencing any pain, thus making it much more suitable for all types of wounds.
BMG dressing’s microfibers absorb fluid from a wound and form a gel-like substance upon contact with wound exudate, thus helping to prevent periwound maceration and making it suitable for low to moderate exudating wounds. As it is in gel form, it helps in maintaining a moist environment, which aids in promoting good granulation tissue formation as shown in all four cases. Nevertheless, other elements play a role in the process of wound healing (Archana et al, 2013). Patient 3 has the lowest percentage of wound size reduction when compared to the other three patients. The slower healing could be attributed to factors such as advanced age and his immunocompromised status. BMG dressing aids in autolytic debridement by moisture-retentive properties, which helps soften nonviable tissue and make it easier to remove during mechanical debridement (Archana et al, 2013).
The BMG dressing provides an optimal moist wound environment, a critical factor for expediting wound healing. It also forms a barrier that protects the wound from external contaminants while permitting passage of oxygen. The gel formation additionally serves to entrap the pathogenic bacteria from the wound site and prevent the dressing from adhering to the wound bed, hence reducing the likelihood of pain and trauma to the wound bed (Archana et al, 2013).
Another observable feature in this case series is the degree of exudate. As per the World Union of Wound Healing Societies Consensus Document, ‘Wound Exudate: Effective Assessment and Management’ (World Union of Wound Healing Societies, 2019), the factors that influence the level of wound exudate are wound aetiology, the stage of wound healing, the size of the wound and the presence of other medical conditions and complications in the patient. Table 2 displays all four cases that demonstrate a decrease in exudate level, as the size of the wound decreases over time.
Limitations
The number of patients was small and, thus, it may require another study involving larger patient numbers and multiple centres in future.
Conclusion
This case series demonstrated that the chitosan-based BMG dressing is an effective adjunct in managing postoperative wounds. All four patients saw a significant reduction in wound size and exudate levels, supporting the BMG dressing’s role in accelerating wound healing, promoting granulation tissue formation and maintaining a moist wound environment. The dressing’s ease of use, biocompatibility and pain-free application further enhance patient comfort and treatment compliance.