Wound healing is a complex biological process in the human body that has four phases: haemostasis, inflammation, proliferation and remodelling. For a wound to heal successfully, all four phases must take place in the right order and for the right duration (Guo and Dipietro, 2010).
Diabetes, a major public health concern in Malaysia, is closely related to increased macro and microvascular complications, as well as premature and preventable mortality. In 2011, the fourth Malaysian National Health and Morbidity Survey (NHMS IV) reported the prevalence of type 2 diabetes increased to 20.8%, affecting 2.8 million individuals compared with the third National Health and Morbidity Survey (NHMS III), which reported a prevalence of 14.9% in 2006 (Hussein et al, 2015). In patients with diabetes the healing process is prolonged regardless of its initial aetiology. The delay in wound healing increases the risk of complications, such as infection, sepsis and amputation (Mieczkowski et al, 2022).
There has been growing interest among researchers in the use of natural products to stimulate wound healing, for instance, Centella asiatica extracts. Centella asiatica, locally known as ‘pegaga’, or more commercially known as ‘Indian pennywort’, is a lightly aromatic, slender and perennial creeper that blooms in shady, marshy and humid areas in tropical and subtropical Asian countries such as Malaysia, India and China (Tan et al, 2021). It has been recommended for the treatment of a variety of skin conditions, such as lupus, eczema, psoriasis, leprosy, and varicose ulcers (Gohil et al, 2010). However, there are reported side effects of Centella asiatica including drowsiness after consuming a high dose, as well as contact dermatitis and skin irritation from topical application (Eun and Lee, 1985; Gomes et al, 2010). It can also cause adverse effects on liver function, when used over many months as the metabolism of its active metabolites (medecassic acid and asiatic acid) slows down, which may produce toxicity (Songvut et al, 2021).
Triterpene compounds: asiatic acid, madecassic acid, asiaticoside and madecassoside are the principal components of Centella asiatica, responsible for wound healing. The action of these active compounds has been demonstrated in a large number of scientific reports involving in vitro and in vivo experiments(Bylka et al, 2013). All triterpene compounds facilitate wound healing by increasing collagen synthesis in human dermal fibroblast cells. Furthermore, triterpenoid asiatic acid is the most potent component of Centella asiatica, induces the expression of tumour necrosis factor-alpha induced protein 6 (TNFAIP6), a hyaladherin involved in extracellular matrix remodelling and modulation of inflammation in human fibroblasts (Maquart et al, 1999).
Studies show that triterpenoid asiaticoside can induce type I collagen by activation of transforming growth factor beta (TGF-β) receptor I kinase (Lee et al, 2006). An in vivo study by Shukla et al (1999), on the activity of asiaticoside in normal as well as delayed-type wound healing, reported increased collagen I synthesis in wound healing, demonstrated by increased tensile strength (a measurement of its load capacity per unit area). Using a guinea pig punch wound model they showed topical applications of 0.2% solution of asiaticoside produced 56% increase in hydroxyproline (p<0.001), 57% increase in tensile strength (p<0.05), increased collagen content and better re-epithelialisation (Shukla et al, 1999).
A study by Liu et al (2008) on triterpenoid madecassoside in vitro demonstrated the ability of madecassoside to promote type I and III collagen synthesis, stimulate the proliferation of cultured human fibroblasts, augment inflammatory cell infiltration, increase angiogenesis and nurture re-epithelialisation.
In cases of persistent inflammation as is the case in chronic/hard-to-heal wounds, madecassic acid and madecassoside triterpenes of Centella asiatica inhibit the inflammatory mediators, thus reducing inflammation. In an in vitro study by Won et al (2010) madecassic acid in Centella asiatica was found to suppress the inflammatory mediators, nitric oxide (NO), prostaglandin E2 (PGE2), tumour necrosis factor-alpha (TNFα), interleukin-1 beta (IL-1β) and interleukin-6 (IL-6) more potently than madecassoside. This was due to downregulating nuclear factor kappaB (NF-KappaB) activation in macrophage cells. This action results in a lower inflammation and allowed the wounds to progress towards healing.
Centis cream containing total triterpenic fractions of Centella asiatica (TTFCA) in form of topical application can modulate the wound healing actions demonstrated by these active components of Centella asiatica especially when anticipating delayed wound healing. Local side effects such as contact dermatitis and skin irritation are possible but rare in ointment preparation of Centella asiatica extract as shown in a case study by Gomes et al (2010).
Objective
To establish if there are any clinical benefits of topical application of total TTFCA (Centis Cream, Phyto Specialities Private Limited) on wound healing.
Materials and methods
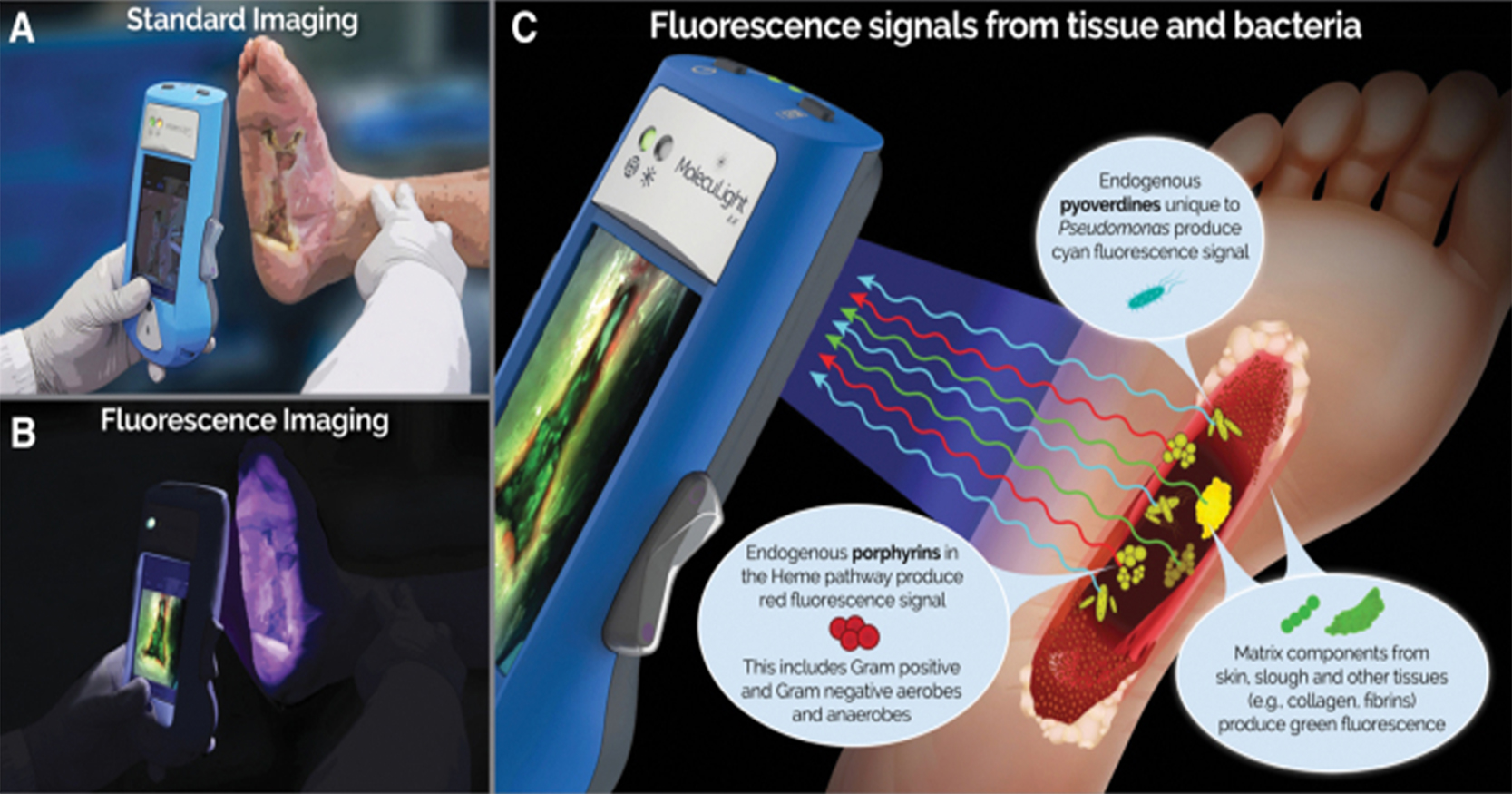
This study took place in the Wound Care Clinic Hospital Kuala Lumpur between September 2019 to November 2019. A convenience sampling method was used. The inclusion criteria was patients with underlying diabetes mellitus who presented with wounds, had a good diabetic control with a latest HbA1C of less than 7% and no episode of hyperglycaemia during wound follow-up. Wounds were assessed using TIME concept and Harikrishna Periwound Skin Classification (HPSC) to determine the status of the wound bed and the condition of the periwound skin (Nair et al, 2020b; Table 1). Only exuding wounds and/or inflammation and without infection, classified within HSPC Class 2 or 3 were included. Based on the study timeline and inclusion criteria, three patients were recruited in this study.
During follow-up visits, patients were assessed as follows:
- All previous dressings were removed from the wounds and any remaining medications were rinsed using sterile water
- The wound bed was cleaned with sterile gauze and any detachable materials were fully removed
- The length and width of the wound bed were measured by using a standardised scale unit
- The measurement of wound size/lesions (length x width) and their healing progress were assessed every time after the dressing was changed
- The wound bed and periwound were assessed on its general condition
- Once the physical assessment was completed, the primary dressing was applied with topical total TTFCA
- Barrier cream was applied to the periwound skin and a secondary dressing of either polyurethane foam or film was used
- The dressing was changed and reviewed in the clinic three times per week (alternating days) until the end of the study.
This study was carried out in accordance with the Declaration of Helsinki’s guidelines and approved by the hospital review board. Patients gave consent to use clinical images and case details for publication/research purposes before the start of the study.
Results
We recruited three patients in this observational study. In terms of demographic data, all patients we recruited by convenience sampling, were male and age 50 years old and above. All three patients had underlying diabetes mellitus with one patient having an additional comorbidity, hypertension.
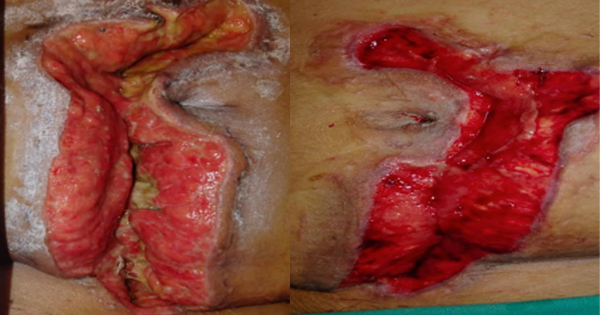
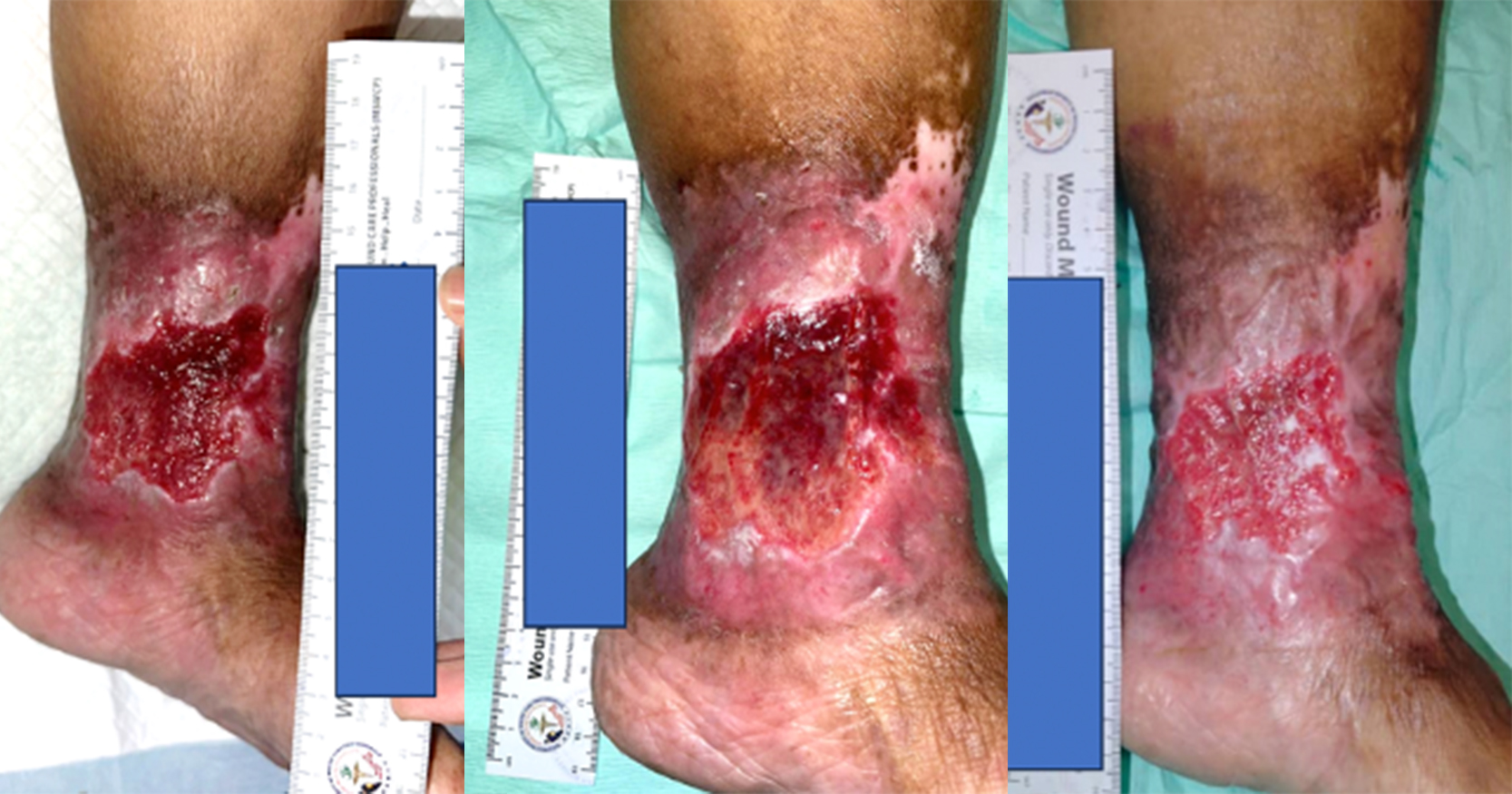
Among the three patients selected, two patients had chronic wounds and one patient has an acute wound. The first patient (Case 1) developed a chronic wound over posterior right ankle after screw fixation surgery due to a calcaneal fracture. Upon starting this study, his wound duration was 8 years since the surgery. The second patient (Case 2) developed an acute diabetic wound over his anterior distal shin of the right lower limb two days before being taken into this study. The final patient (Case 3) had a delayed wound healing after carbuncle saucerisation surgery over his upper back.
The three wound cases recruited in this study at Wound Care Clinic in Hospital Kuala Lumpur and shown in Table 2. At the end of the study, all three patients showed a wound size reduction while maintaining a good wound bed condition (healthy granulation tissue) and re-epithelialisation of the wound edge. Wound size reduction in three patients ranged from 12.5–100%. Out of these 3 patients, 2 patients achieved wound closure (Case 2 and Case 3).
Discussion
Topical application of TTFCA mainly acts to reduce inflammation, increase angiogenesis, enhance extracellular matrix remodelling and promote collagen synthesis at the wound site. Delayed wound healing may occur because of prolonged inflammation at the wound site, which can prevent the next phase of the wound healing process. Biologically active components of TTFCA, Madecassoside and madecassic acid, suppress the inflammatory mediators and increase angiogenesis, which should push the wound on to a normal healing trajectory (Won et al, 2010). Other TTFCA compounds, especially asiaticoside and asiatic acid, enhance the extracellular matrix and stimulate collagen synthesis during the proliferation and remodelling phases of wound healing, assisting wound closure (Gohil et al, 2010).
In this observational study all three patients with underlying diabetes showed wound size reduction, two of which achieved wound closure by the end of this study. Despite these two patients having underlying diabetes mellitus, wound closure was faster in the patient with an acute wound as shown in Case 2 (22 days), compared with the chronic wound in Case 3 (35 days). This finding is in agreement with an in vivo study done by Shukla et al (1999) on the effect of asiaticoside on punch wounds in streptozotocin-induced diabetic rats, where healing was delayed. In streptozotocin-induced diabetic rats, topical application of 0.4% solution of asiaticoside (one componant of TTFCA) over punch wounds increased hydroxyproline content, tensile strength, collagen content and re-epithelialisation, thereby facilitating wound healing.
Case 1, a chronic wound, had the smallest wound size reduction of 12.5%. This might be affected by the duration of the wound, location of the wound and patient’s footwear. This patient had the longest duration wound (8 years) at the start of the study compared with the other two patients. This may have resulted in the slower healing rate. The wound was located at the posterior aspect of the ankle joint overlying the Achilles tendon, which is involved in active ankle movement during walking. This might cause repetitive stretching of the wound area and delay healing. Furthermore, the wound location in Case 1 is affected by persistent pressure from the heel counter of the patient’s shoe especially during walking. Therefore, prescription of custom molded shoes is required to accommodate, stabilise, and support deformities while limiting inappropriate motion of joints (Baumhauer et al, 1997). The wound locations of the other two patients are at anterior distal shin and posterior upper back respectively. These are neither at common pressure injury sites in ambulating people nor at body joints thus there is less active body movements.
Limitations
Limitations of this study include lack of patients recruited as there were only three patients in this pilot study and the non-standardised treatment length. Furthermore, chronic wounds classified as Class 4 and 5 according to HSPC were not included as more aggressive treatment would be required. Robust multicenter trials with larger sample size are required to evaluate the effect of this plant-based cream in wound management especially in chronic complex wounds.
Conclusion
This case series study demonstrated the clinical efficacy of TTFCA in topical application (Centis Cream). Effective wound size reduction was observed in all three patients with two patients achieved wound closure. Moreover, TTFCA was shown to be effective in wound healing and closure in both an acute and chronic wounds. The selective action on wound tissue and simple treatment of the topical plant-based application has the potential to be valuable in wound care management but much larger studies are required to support this assertion. This suggests that TTFCA is able to provide a clinical benefit in routine acute and chronic non-infectious wound management.