Osteomyelitis pubis is a rare condition, resulting from infection of the pubic symphysis, which accounts for less than 1% of all osteomyelitis cases (Alqahtani et al, 2014). Pathogenesis of this disease is unknown but associated with female incontinence surgery, athletic activity, pelvic malignancy, and intravenous drug user (Ross and Hu, 2003). This condition often has a delayed diagnosis or is mistreated because of the non-specific clinical symptoms (Pauli et al, 2002). The symptoms are suggestive of a differential diagnosis of acute abdomen, urological or gynaecological diseases (Pauli et al, 2002). The patient usually presented to the emergency department with sudden onset of suprapubic pain. A vigilant emergency physician may capture the condition with a more thorough investigation.
A culture-specific therapeutic antibiotic regime is essential for treating pubic osteomyelitis, and surgical debridement is required if antibiotic treatment fails (Pham and Scott, 2007). Here we present a case of pubic osteomyelitis, which was initially misdiagnosed and treated as acute cystitis and progressed into abscess formation in the pubic bone.
Case report
A 61-year-old Malay woman with type 2 diabetes presented with a one-month history of suprapubic pain accompanied by intermittent fever. The pain was spontaneous in onset, without any history of trauma, sport injury or previous infections, such as upper respiratory tract infection, dysuria, or an infected wound. A federal hospital had previously diagnosed her with acute cystitis, one week after the onset of symptoms, and administered two weeks of intravenous antibiotics. Despite completing the course of antibiotics, she continued to experience pain in the suprapubic and pubic regions, which hindered her mobility. Her pain radiated from the pubic region to the medial aspect of both thighs, with the left thigh being more affected by movement. A week before her presentation, her pain increased to the point that she became bedridden. The patient’s abdomen was soft, but the suprapubic region, pubic bone, and bilateral inguinal regions were tender. The inguinal lymph nodes were palpable and painful bilaterally. Pain reduced the active and passive range of motion of both hips.
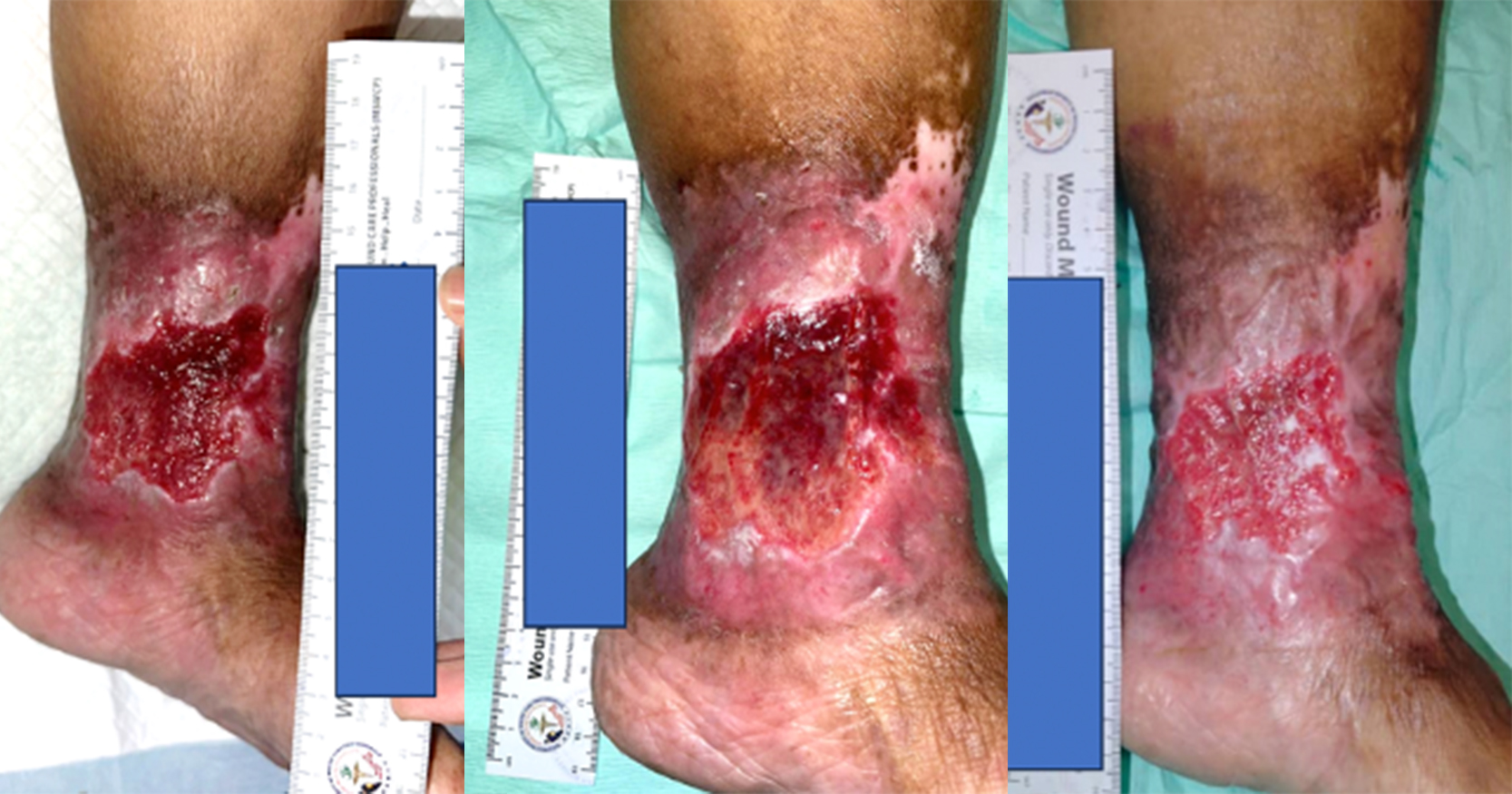
Her leukocyte count was 15.4×109 cells/L (normal range: 4–11 x109 cell/L), with polymorphonuclear leukocytosis being predominant. C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) were each 316.0mg/L and 66.0mm (normal levels based on age: CRP <5.0 mg/L; ESR 35.5mm). Urine examination and microscopic examination (FEME) results were negative, with no signs of a urinary tract infection (UTI). Urine cultures were also negative. Radiographs of kidney, ureter, and bladder (KUB) revealed no osteolytic changes (Figure 1). Due to the limited availability of MRI slots, a contrast computed tomography (CT)-scan of the pelvis was requested as an emergency. It revealed a rim-enhancing collection that measured 1.2 x 1.7 x 2.5cm (anteroposterior–AP; width–W; craniocaudal–CC) at the insertion site of the rectus abdominis, as well as bone erosion of the pubic symphysis (Figure 2). The empirical antibiotic treatment began with 1.5g of Cefuroxime three times a day administered intravenously. Blood culture result revealed meticillin-susceptible Staphylococcus aureus (MSSA). The patient was referred to an infectious specialist, and the medication was changed to IV Cloxacillin 2g four times a day.
After two weeks, a second contrast-enhanced CT of the pelvis revealed an expanding soft tissue abscess at the base of the rectus muscle with extension to the left pectineus muscle, as well as worsening osteomyelitis of the pubic symphysis and both superior pubic rami. The collection expanded to 5.4 × 4.2 x 5.9cm (AP x W x CC) and revealed more fluid density areas with visible air pockets (Figure 3). A biopsy and drainage guided by a CT were performed (Figure 4), however, attempts at aspiration were futile. We performed four biopsies of soft tissue, and the samples were sent to the laboratory for culture and sensitivity, histopathological examination and Mycobacterium tuberculosis culture. The culture was negative; the histopathological examination demonstrated acute chronic inflammation, and no Mycobacterium tuberculosis was found.
The pain improved with analgesics, and the patient began to walk with a walking frame three weeks after receiving antibiotics. Repeated biweekly tests of infectious indicators showed a decreasing trend, with the CRP reduced to 33.14mg/L and white cell count reduced to 8.7 x 109 cells/L. A repeat blood culture one week later revealed no growth. After three weeks of intravenous Cloxacillin, three weeks of oral sulfamethoxazole/trimethoprim 1200/240mg was prescibed twice a day. This completed a six-week course of antibiotics. No growth was seen in repeated blood cultures six weeks after the administration of antibiotics. At a three month clinic follow-up, the patient’s pain had disappeared, infection marker CRP had reduced to 11.19mg/L and the white cell count was reduced to 6.9×109 cells/L. She had resumed all her normal activities. A one-year follow-up revealed no recurrence.
Discussions
Infection of the pubic symphysis is rare. Osteomyelitis pubis is an infection of the pubic symphysis that has an unknown aetiology. (Knoeller et al, 2006). Osteitis pubis was the inflammatory counterpart of pubic symphysis and was more prevalent than pubic osteomyelitis. Edwin Beer defined osteitis pubic as a self-limiting inflammatory condition of the pubic symphysis in 1924 (Pham and Scott, 2007). It was more prevalent among young adults between the ages of 35 and 49, with a male predominance, and its cause was unclear (Pham and Scott, 2007). Both conditions are hard to differentiate until the conservative treatment of osteitis pubis fails (Pham and Scott, 2007).
Suprapubic pain, fever, painful waddling, and antalgic gait were common pubic osteomyelitis symptoms (Ross and Hu, 2003). Rectus and adductor muscle spasm may cause groin or lower limb adductor muscle pain, as well as forward bending while walking (Knoeller et al, 2006). Clinical findings may reveal tenderness of the pubic bone, including superior and inferior pubic rami and inguinal lymphadenopathy (Ross and Hu, 2003; Pham and Scott, 2007). The two primary causes of pubic symphysis are thought to be blood-borne mechanisms that lead to subsequent septic seeding during bacteraemia and the direct inoculation of bone during surgery (Becker et al, 2020). Pubic osteomyelitis risk factors included urological surgery, female incontinence surgery, athletes, particularly those participating in sports requiring forceful hip adduction, a history of pelvic cancer, and intravenous drug use (Ross and Hu, 2003). Other risk factors include invasive pelvic surgery, pregnancy or childbirth, gracilis-adductor tendinopathy, diabetes and hematogenous seeding from infective foci on other body parts (Anisau and Vanhoenacker, 2017). The remaining 10% has no identifiable aetiology or risk factors. The causal organism may vary according to risk factors, however Staphylococcus aureus is the most prevalent pathogen that causes osteomyelitis pubis (Ross and Hu, 2003).
In the early stages of pubic osteomyelitis, a pelvic radiograph may not be useful for diagnosing the illness. A pelvic CT scan has a sensitivity of 90% and can reveal symphyseal widening, abscess collection, osteolytic bone abnormalities, and irregular joint surfaces. MRI provides the highest sensitivity, 100%, according to Ross and Hu (2003). However, Becker et al (2020) stated that CT scans were more accessible and 100% accurate at confirming the diagnosis.
Pubic osteomyelitis can be treated with a minimum six-week course of antibiotics (Ross and Hu, 2003). Foreign bodies, such as bone anchors used in incontinence surgery, or the presence of complications such as pelvic diathesis, bone necrosis, cystic perforation, pelvic instability, and worsening pain that did not respond to antibiotics are indications for surgical treatment by debridement and bone curettage (Ross and Hu, 2003; Pauli et al, 2002). Mortality of pubic osteomyelitis was reported as 2% (Ross and Hu, 2003).
In our case, the diagnosis of pubic symphysis osteomyelitis was made swiftly with the use of a contrast CT scan of abdomen, as it was easier to access than an MRI. Even though the patient presented with typical suprapubic and pubic pain symptoms with radiation to the adductor compartment of the thigh, an inattentive physician or surgeon could miss the diagnosis of osteomyelitis pubis. With an established diagnosis from the CT scan, the physician could immediately begin the appropriate treatment. The patient presented with a blood-borne acute presentation of pubic symphysis osteomyelitis with spontaneous onset of symptoms and no previous risk factors or surgical history, for which Cloxacillin was administered intravenously based on blood culture and sensitivity results indicating MSSA. Despite this, the repeated contrast CT scan after two weeks of antibiotic treatment revealed that the collection in the pubis bone had grown in size. As the patient’s symptoms improved with the administration of antibiotics, surgical intervention was withheld. Although the CT-guided aspiration was unproductive, the negative growth observed in the biopsied tissue culture indicates that antibiotics effectively eradicated the infection. With the involvement of an infection specialist, our patient was successfully treated for osteomyelitis pubis with a six-week course of antibiotics containing cloxacillin and sulfamethoxazole/trimethoprim. She recovered without complication or recurrence, and resumed her normal daily activities following a three-month clinic checkup.
Limitation
This case report has several limitations to consider. Due to the rarity of this condition, the report is based on a single patient, which limits the generalisability of the findings to a larger population. The response of a patient to a particular treatment or intervention can vary, and it is possible that the outcomes observed in this case are not representative of other patients with comparable conditions. Without a control group of patients who did not receive the same intervention, it is difficult to determine the intervention’s contribution to the observed outcomes. It may be difficult to attribute the observed effects exclusively to the intervention being evaluated if factors such as spontaneous remission or natural disease progression confound the results. In addition, the retrospective nature of this case report raises the possibility of recall bias. The data was derived from the patient’s medical records that may be insufficient. In this case report, the duration of follow-up (one year) was relatively brief. Long-term outcomes and potential complications may arise after a more extended period were not explored. In light of these limitations, additional research, such as well-designed clinical trials with larger sample sizes and suitable control groups, is required to validate the findings and establish solid evidence.
Conclusion
Osteomyelitis pubis is a rare condition that requires a high level of suspicion in its diagnosis. A CT scan could have aided in establishing the diagnosis earlier. Blood-borne aetiology can be adequately treated with intravenous antibiotics followed by oral antibiotics for a minimum of six weeks. If conservative treatment fails to improve patient outcome, surgical intervention is necessary.